
Snoring and sleep disorders affect up to 70 million Americans. The mouth-body connection allows your dentist to pick up the first signs of the mouth.
Sleep apnea symptoms can increase the risk of heart and brain disease. If you snore, how can you find out if you have sleep apnea? Not all snoring and sleep disorders mean you have sleep apnea.
The two types of sleep disorders we’ll talk about are:
- Obstructive sleep apnea (OSA)
- Upper airway resistance syndrome (UARS)
Obstructive sleep apnea is much easier to pick up. It almost always accompanies snoring and is found with a sleep test.
Upper airway resistance syndrome, on the other hand, isn’t defined as a medical term. Many people don’t know it exists. UARS can present silently without snoring. People at risk are a different group to obstructive sleep apnea. It includes females, with a slender build, and day-time sleepiness.
Here is a list of symptoms, that often accompany sleep disorders. The easiest to spot are snoring or daytime sleepiness. Each of these means it’s time to see your physician or sleep, focused dentist.
Common conditions associated with sleep disorders:
The digestive system
- Irritable bowel syndrome
- Crohn’s disease
- Chronic diarrhea
- Constipation
- Indigestion
- Acid reflux
- Bloating
Low blood pressure
- Cold feet and hands (low oxygenation)
- Socks and mittens all year round which is also known as Raynaud’s phenomenon.
- Dizziness
- Lightheadedness and fainting (23% with UARS have low blood pressure)
Ears, nose, and throat
- Sinus pain
- Sinus headaches
- Migraines
- Tension headaches
- Deviated septum
- Chronic blocked sinus
- Inferior turbinate hypertrophy
- Nasal valve collapse
Stress
- Poor or light sleep
- Teeth clenching
- Cheek or tongue biting
- Depression
- Anxiety
- ADHD in children
Tests for sleep disorders: Polysomnography (PSG)
The most accurate measure of sleep disorder is a polysomnography (PSG). It’s a test that measures breathing and vitals for an entire night of sleep. A PSG records the amount of time airflow stops for at least 10 seconds. You might have heard someone who snores experience an apnea. It’ a pause between breaths.
The PSG will give a measure in known as the Apnea Hypopnea Index (AHI). Another measure is the respiratory disturbances index (RDI)
AHI Score: this is the average number of apneas (more than 10 seconds) and hypopneas per hour.
RDI Score: average number of respiratory disturbances. These include obstructive apneas, hypopneas, and respiratory event–related arousals [RERAs]) per hour.
No consensus exists for AHI or RDI to be the standard index to diagnose sleep apnea for insurance.
AHI Score:
0: healthy
0-5: normal
5-15: Mild obstructive sleep apnea
15-30: Moderate obstructive sleep apnea
31+: Severe obstructive sleep apnea
These scores state the severity of obstructive sleep apnea.
Oxygen Desaturation
Reductions in blood oxygen levels (desaturation) are recorded during polysomnography. Normal blood oxygen level (saturation) is usually 96 – 97%.
O2 Desaturation Measures:
Mild: reductions to not less than 90%
Moderate: the 80 – 89%
Severe: below 80%
The range from mild, moderate to severe sleep apnea shows the level of oxygen deprivation. The class is important, but even if you’re at the lower end of the scale, there can be health risks.
Diagnosing Upper Airway Resistance Syndrome
The problem with UARS is that it is a relatively new condition. It’s not a defined medical term yet. People with UARS also have an AHI of 0. That means a PSG sleep test shows they don’t stop breathing, and often don’t snore.
There is currently no test to diagnose upper airway resistance syndrome. There are however many different measures from a PSG and other techniques.
Upper airway resistance syndrome is truly defined by increased pressure in the airway.
Here is a set of tests that can help determine sleep disorder or UARS:
ESS: Epworth Sleepiness Scale, Pes: Esophageal pressure,
AHI: Apnea / Hypopnea Index,
RERA: Respiratory Event-Related Arousal,
RDI: Respiratory Disturbance Index
Pes: Esophageal pressure
Flow limitation: Nasal cannula
The Epworth Sleepiness Scale (ESS) is a series of 8 questions. Respondents are asked to rate, their level of sleepiness on a day to day basis.
A score above 9 (higher than average daytime sleepiness, often seen in UARS.
Respiratory effort related arousals (RERAS) are a measure of efforts to breathe.
The Respiratory Disturbance Index (RDI) can measure these efforts. The RDI includes not only apneas and hypopneas, but may also (RERAS). This means a person’s RDI can be higher than his or her AHI.
An important measure is an esophageal pressure, measured by esophageal manometry (Pes).
Negative esophageal pressure is the hallmark of UARS. One tool to measure this is flow limitation by nasal cannula. These aren’t included in a standard polysomnography.
In 2012 Pepin et al defined a diagnosis for upper airway resistance syndrome.
- Excessive daytime sleepiness (ESS) > 9
- Negative esophageal pressure (Pes) – (not given in standard PSG test)
- Flow limitation by nasal cannula
- RERAs more than 50% of respiratory events
There has been no consensus on the true diagnoses of UARS yet.
Remember that every test is one measure of your sleep disorder. You can use it as a guide to compare with your sleep test results.
You will need to talk to your physician about your particular case.
Ear nose and throat (ENT) assessment
The location or restriction in your airway is also important. An ENT will determine where your restriction is occurring. They will perform an endoscopy to examine nasal airways, adenoids, and tonsils.
Chronic blocked sinus may have the following symptoms for 12 weeks or more:
- Facial pain/pressure
- Facial congestion/fullness,
- Nasal obstruction/blockage,
- Thick nasal discharge/discolored post-nasal drainage
- Pus in the nasal cavity, and at times, fever
- Headache, bad breath, and fatigue.
Areas of blockage or limited airflow
- Nose – deviated septum
- Nasal Sinus
- Lower back of throat or bottom of your neck.
Visual assessment of size of airway
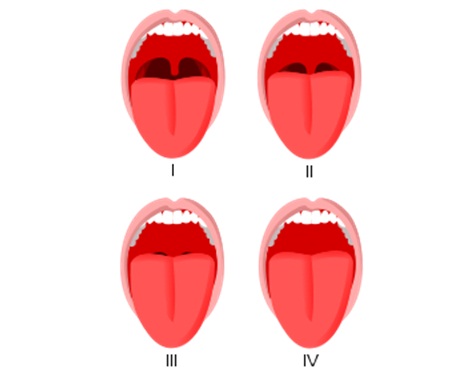
Your GP or dentist can make an assessment of your tongue blockage with the Mallampati score. It’s assessed in a sitting posture with open mouth and protruded tongue as far possible.
The risk of OSA increases by 1.5 fold as Mallampti score increases.
Sleep tests can be confusing. This guide should help you understand the tests available for sleep disorders.
Can you cure sleep apnea? Treatments for sleep disorders
Treatments for OSA and UARS are currently the same.
Continuous positive airway pressure (CPAP)
CPAP is a machine you wear at night that uses pressure to push the airways open. For severe cases of obstructive sleep apnea, it can be effective, reducing high blood pressure. However long-term compliance rate is poor at 54%.
For upper airway resistance syndrome, the success is generally because of low compliance.
Mandibular Advancement Splint (MAS)
This is a type of night splint made for teeth grinding. Made by your dentist, it holds the lower jaw forward when you sleep. It is designed to stop the tongue from falling back into the throat causing RERAs or apneas.
Research has shown it to be as effective as CPAP in certain situations. However, OSA caused by nasal restriction will respond poorly to MAS.
ENT assessment should always precede MAS therapy.
ENT Surgery
Otorhinolaryngologist (ENT) assessment of nasal breathing includes deviated nasal septum and turbinate hypertrophy.
In certain cases, medication or surgical intervention may improve sleep disorders.
ENT disorders are more common in OSA and UARS, assessment is crucial.
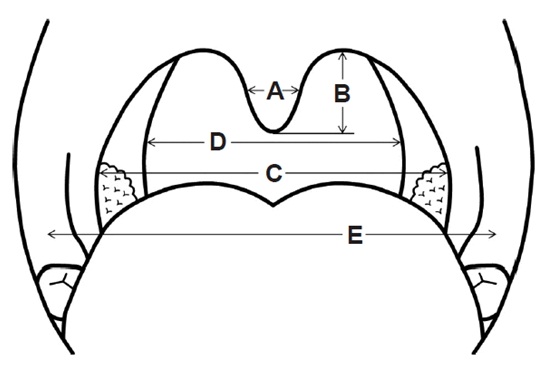
Expansive palatal orthodontics
Adult palatal orthodontics can help to increase volume in the airways and reduce OSA.
This is a relatively new field. Early signs show big potential to cure sleep apnea and sleep disorders.
Have you experienced sleep apnea symptoms? Let us know your experiences in the comments.
Myofunctional therapy
A myofunctional therapist or orofacial myologist helps to retrain oral and breathing habit. This includes training nasal breathing, correct tongue posture, and closed lip habits. There is early evidence to suggest that myofunctional therapy is effective alongside other sleep apnea treatments.
Do you suffer from snoring or sleep apnea? Did these solutions work for you? Leave your comments in the section below.
For more information on Dr. Lin’s clinical protocol that highlights the steps parents can take to prevent dental problems in their children: Click here.
Want to know more? Dr Steven Lin’s book, The Dental Diet, is available to order today. An exploration of ancestral medicine, the human microbiome and epigenetics it’s a complete guide to the mouth-body connection. Take the journey and the 40-day delicious food program for life-changing oral and whole health.
Click below to order your copy now:
US AMAZON
US Barnes & Noble
UK AMAZON
Australia BOOKTOPIA
Canada INDIGO



3 Responses
I didn’t realize that snoring and sleeping disorders affected 70 million Americans. That blows my mind that there are so many of us out there. I have struggled with some and I think that it’s finally time to get it taken care of. I think that I’ll see a doctor about what my options are for dealing with what is wrong.
Thanks for the information on how a sleep disorder can affect your life and how you can test for it. I had no idea that you could tell a sleep disorder from something like your blood pressure. I would imagine that getting a nice rest at night could really make a big difference throughout your day.
It sure is nice to know that sleep tests are capable of diagnosing sleep apnea and other sleeping disorders. My eldest son snores very loudly, so much so that it has got me worried about his health. Sleep apnea is not something that should be taken lightly, so I’ll be sure to get him into a sleep test as soon as possible.